The Procedure
The Latarjet procedure involves transferring a part of the shoulder blade bone called the coracoid process to the glenoid. The surgery is usually done in people who have an unstable shoulder where dislocation occurs at the front of the shoulder. The typical indications for surgery are recurrent anterior shoulder instability in patients engaged in contact sports and who have bone loss from the glenoid, or in patients with recurrent instability after failed shoulder surgery.
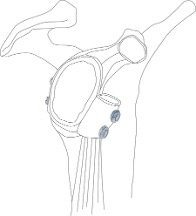
The Latarjet procedure is a complex shoulder surgery that I perform arthroscopically. It involves transferring the coracoid process from the top of the shoulder blade to the front of the glenoid. This stabilises the shoulder joint and prevents further dislocations. During the surgery, the subscapularis muscle, which runs across the front of the shoulder, must be split to allow the bone block to pass through and be attached to the glenoid.
In traditional Latarjet surgery techniques, the anterior capsule of the shoulder joint is ablated and thus the anterior labrum (the ring of cartilage that surrounds the shoulder socket) is not repaired. I have developed a modified arthroscopic technique where the anterior labrum is preserved and repaired during the Latarjet procedure.
Complications
General risks of surgery include:
- Bruising & haematoma: this will vary for each patient. Bruising is a normal side effect of surgery and usually resolves in a short time.
- Infection: infection is a rare but possible risk and is usually treated with antibiotics.
- DVT and PE: deep vein thrombosis and pulmonary embolism are blood clots that form in either the lower limbs or lungs. If left untreated, DVT and PE can have serious effects, however if treated promptly, the risks are significantly lowered. More information can be found here
- Anaesthetic risks: general anaesthetic (GA) carries a number of risks, which will be discussed in detail with your anaesthetist prior to surgery. Fortunately, Australia is one of the safest places to undergo a GA. In Australia, the risk of mortality from GA is around 1 in 100,000. For context, the risk of death in a car accident in Queensland is around 1 in 10,000 per year.
- Wound issues: some superficial issues can develop in surgical wounds postoperatively, however most will require a small intervention to resolve the problem.
Risks and complications specific to the Latarjet and labral repair surgery include:
- Recurrent instability: Around 2 to 4% of patients find that the shoulder joint still feels unstable after Latarjet surgery, though rarely do patients experience further dislocation postoperatively.
- Shoulder stiffness: this can occur after surgery, developing from scar tissue or residual frozen shoulder. In about 2% of patients, I perform an arthroscopic release of the shoulder at 12 months after the initial surgery to restore the range of motion to the shoulder.
- Hardware issues: screws or other hardware used in the surgery may cause issues.
- Nerve injury: the risk of severe nerve injury is around 1 in 200, which could require a nerve repair or nerve transfer.
- Issues with the bones & graft issues: the bone block can fail to unite to the glenoid, as well as fractures.
- Frozen shoulder: this involves pain and stiffness in the shoulder, and resolves over time on its own accord.
Pre Op
Whilst you wait for your surgery date, there are a few things to do:
- Speak to your health fund to confirm if the hospital fee for your surgery is covered on your policy
- Speak to your anaesthetist to confirm their fees
- Register your details with the hospital
- Read through, complete and return your paperwork to my office
- Plan your transport to and from the hospital. You won’t be able to drive yourself home after the surgery, so make sure you have a travel plan in place
- If required, arrange any recommended pre op physio appointments
- If required, get any pre op pathology tests (e.g., blood tests)
- Use benzoyl peroxide 5% wash on your shoulder for 5 applications: twice a day for two days, and then again on the morning of the surgery. This will help reduce your risk of infection from Cutibacterium acnes.
- Pack a bag for your hospital stay including regular medications in the original packaging, a loose button-up shirt to wear after surgery, nightwear, personal items including toiletries. If you have sleep apnoea, you must bring your CPAP machine.
- If you are on any blood thinners, ring my office and confirm when to stop taking them before the operation.
- If you are on any diabetic tablet medications, ring your anaesthetist and confirm whether you need to stop taking them before the operation
- Confirm your admission details with my office one to two business days prior to surgery
Though this can seem overwhelming, you will be provided with detailed instructions on what needs to be done so your surgery journey can be as smooth as possible.
Day of Surgery
Your admission details will be confirmed one to two business days prior to surgery. You will need to make note of your admission time and your fasting time. Your admission time may be as early as 6am. If you aren’t local to Brisbane, it is usually recommended that you stay the night before in case your admission is early.
When you arrive at the hospital, you will go through the admissions process and then be taken through to the surgical waiting area. Your anaesthetist will have a short consultation with you before you go into theatre and under general anaesthetic. I will say hi to you before the surgery in the anaesthetic bay of the operating theatre and mark your operation site with you.
Your hospital stay will usually be one night. You will have an Xray of your shoulder the next morning. The nurses will change your dressings and you will be discharged usually around 10am. I will see you before your discharge. I will provide you with a folder containing a detailed postoperative pack including a letter telling you what I found at surgery and exactly what I did in your operation along with information about your rehabilitation and postoperative care. Remember to have someone available to take you home from the hospital.
Post Op Recovery & Healing
Getting adequate rest is essential for a good recovery after Latarjet surgery. In the first 6 weeks after surgery, resting is more important than exercise. The main movement that must be avoided during recovery is an active biceps contraction, which is what happens when lifting an object towards your head by flexing your elbow. In the Latarjet procedure, the biceps tendon is attached to the bone block, which has been transferred to the front of the shoulder. If your biceps contracts and pulls on the transferred bone block during your recovery, this will prevent the bone block from healing completely, or dislodge it from its position. Therefore, a sling will need to be worn full time for six weeks after surgery. You won’t be able to drive, or work, or do your normal physical activities during this period, so this must be considered when planning your surgery and throughout your recovery.
The morning after surgery, you will be seen by a physiotherapist who will run through how to go about your daily life and activities in the sling. These will include how to wear your slight, how to get dressed, how to shower, etc.
At six weeks after surgery, a CT scan will need to be performed to confirm bone healing has occurred. If the bone block has healed, then the rehabilitation programme, return to work and sports plans can be upgraded and returning to work and sports can be considered.
Rehabilitation
After Latarjet surgery, rehabilitation will involve strengthening the rotator cuff, and getting proprioception back to a pre-surgery level, as well as immobilisation by wearing a sling for six weeks after surgery. Part of the rehabilitation process involves maintaining strength and conditioning prior to surgery, so that post-op rehabilitation can be effective.
An important factor after surgery is protecting the bone block and allowing it to heal properly, therefore the biceps muscle must not be active. Avoiding active elbow flexion means that bending your elbow will need to be done passively.
While the elbow flexion must be avoided, rehab exercises will focus on external rotation and forward flexion to ensure that the shoulder isn’t tight, and movement is optimal. Usually around three to four weeks after surgery, you can start gentle exercise like walking.
After six weeks, the sling is usually no longer needed, and strengthening exercises can be commenced. There will be some muscle deconditioning in those first six weeks postop, so using a number of strengthening exercises is encouraged.
At 12 weeks after surgery, your range of motion will be assessed. Strengthening the shoulder is once again the main goal, as well as building confidence to restore the maximum range of motion.
The next routine follow up will be at 12 months.
Physiotherapy Guidelines
Day One Physio Guidelines
- The hospital physio will demonstrate how to fit your sling and how to eat, shower & dress whilst in your sling. Please make sure you go through these things with the physio so that you get them really clear in your mind before you leave hospital.
Goals:
- Protect bony healing of transferred coracoid process to the anterior glenoid by limiting active biceps and use of sling for 6 weeks.
- Maintain GH (glenohumeral) Joint ROM (range of motion)
- Sling: to be worn full time for 6 weeks, except while showering and doing prescribed exercises. Check fit, demonstrate activities of daily living (showering, dressing etc)
- Precautions: Avoid any active elbow flexion during Phase I: i.e., no contraction of short head of biceps which will load the coracoid process and may impact bony healing
Therapy:
- Ensure appropriate sling fit, patient taught to don/doff sling independently, hand to align to body midline i.e., fingertips to belly button
- Ensure appropriate sling fit, good posture in sling and scapular awareness.
- GHJt (glenohumeral joint) passive ROM (range of motion) exercises: ER (external rotation) to 30 degrees, Flexion to 120 degrees
- Maintain range of motion of adjacent joints:
- CSp (cervical spine) - full active ROM (range of motion)
- Elbow - No active flexion, ROM (range of motion) exercises: active extension/passive flexion, active pronation/passive supination
- Hand - full active ROM (range of motion)
- Scapula postural awareness and patterning through shoulder ROM (range of motion)
- Therapist to spend time teaching patient not to actively contract biceps with passive elbow flexion, supination activities within sling and forceful grip
- Sling in shower for 2 weeks – patient will require collar and cuff.
- Can work on core, lower limb strength as long as no load on biceps and patient remains in sling
Results After Surgery
Latarjet surgery generally has positive results for stability and movement. There is a low rate of less than 1% for recurrent shoulder dislocations, and most patients report a return to pre-injury levels of activity and range of motion. Long term, however, some patients may develop arthritis.
Around 2 to 3% of patients may develop a tight external rotation, and around 2% report the shoulder feeling a little loose. Further surgery in the way of a Remplissage procedure may be required in some rare instances.
